During today’s noon report, we discussed an interesting case of hyponatremia secondary to adrenal insufficiency. Hyponatremia can be a complex topic, but, as with many topics in internal medicine, a systematic approach can help us understand and manage it effectively.
You can checkout the full slides here
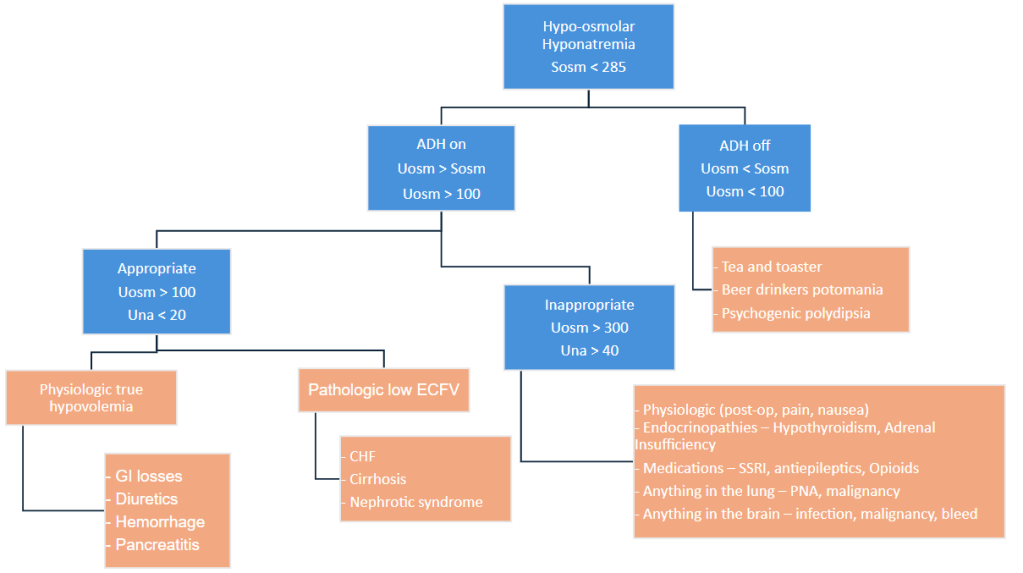
Below is my approach to thinking about hyponatremia:
Here are some additional key takeaways:
- Hyponatremia is a water problem, not a sodium problem! Therefore, it is best understood as a state of “too much water” as opposed to “too little sodium”.
- Understanding hyponatremia requires an understanding of two key hormones: ADH (antidiuretic hormone) and aldosterone, and their roles in sodium physiology. Urine studies, including measurements of urine osmolality and urine sodium, provide insight into the activity of ADH and aldosterone and their effects on sodium levels.
- It’s crucial to distinguish between acute and chronic hyponatremia, as this affects your management strategy. If you’re uncertain whether the hyponatremia is acute or chronic, assume it is chronic.
- Adrenal insufficiency can be a cause of hyponatremia and can be screened by measuring morning cortisol levels. Further evaluation with ACTH (adrenocorticotropic hormone) tests can help determine the specific level of the HPA (hypothalamic-pituitary-adrenal) axis that is affected, aiding in the diagnosis of adrenal insufficiency.




Leave a comment