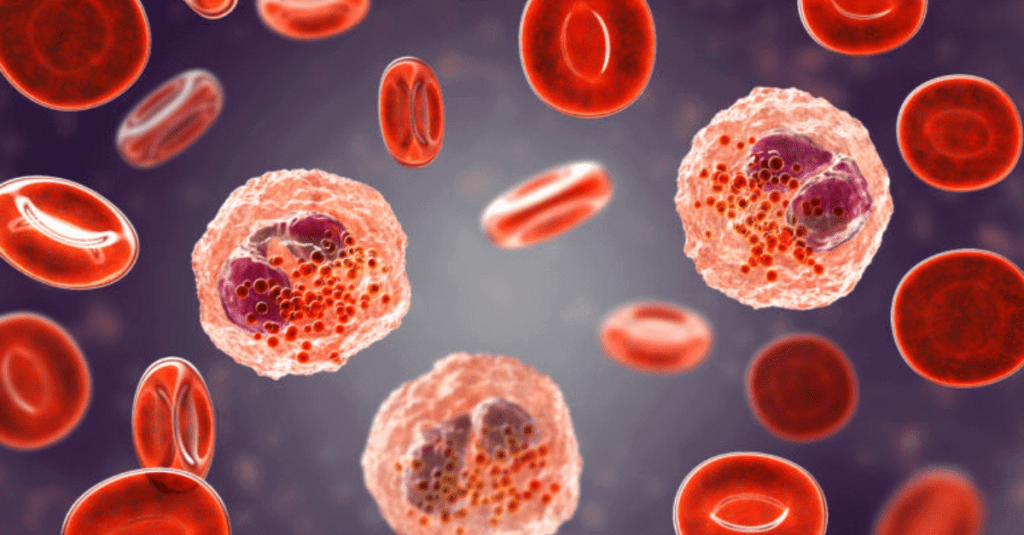
In today’s noon report, we review the topic of eosinophilia, which can have a daunting differential if you’ve never encountered it before!
The case involves a 70 year old woman who presented to the GIM Clinic with 6 weeks of constitutional symptoms and was found to have new anemia (Hb 80) and peripheral eosinophilia (2.6). She had recently returned from a long trip to the Philippines (where she grew up). After extensive workup, she was found to have acute schistosomiasis syndrome!
Please see didactic slides for the report here.
Key takeaway points:
- Hypereosinophilia (absolute eosinophil count AEC > 1500) can be associated with organ dysfunction due to tissue infiltration of eosinophils, release of toxic granules, and release of inflammatory cytokines/ chemokines.
- Degree of peripheral eosinophilia does not always correlate with amount of tissue injury!
- Eosinophilia can be primary (clonal proliferation of eosinophil lineage), reactive (more common), or idiopathic
- Differential:
- Allergic: asthma, allergic rhinitis, atopic dermatitis, eosinophilic esophagitis
- Drug hypersensitivity reactions: DRESS, acute interstitial nephritis
- Infectious: *think parasites!* helminths (strongyloides, trichinella, filariasis, toxocariasis, schistosomiasis etc), scabies, protozoans, fungi (coccidiodomycosis, ABPA (hypersensitivity reaction to aspergillus and not a true infection), histoplasmosis etc), viral (HIV)
- Immune: EGPA, connective tissue diseases, IgG4-related disease, sarcoidosis, and some primary immunodeficiency syndromes
- Malignancy: primary hypereosinophilic syndromes, acute or chronic eosinophilic leukemia, CML, systemic mastocytosis, B and T-cell lymphomas/ leukemias, some solid organ tumors
- Idiopathic: idiopathic hypereosinophilic syndrome
- Miscellaneous: radiation, cholesterol emboli, hypoadrenalism



Leave a comment