Today’s noon report worked through the case of a 78 year old man with a history of pontine stroke, dyslipidemia, hypertension, and T2DM who presented with 3 weeks of progressive, symmetric proximal muscle weakness and a CK of 14 000. He was eventually diagnosed with statin-induced immune-mediated necrotizing myopathy!
See the didactic slide deck here.
Key take home points:
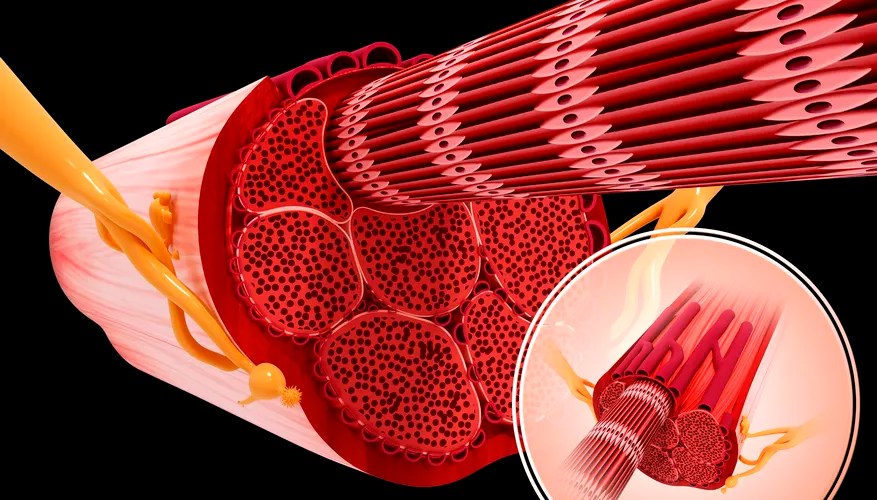
- Approach to weakness (broadly) and elevated CK
- Immune-mediated myopathies
- Investigations and diagnosis
- Clinical history and physical
- Labs: CK, ANA, ENA, myositis autoantibodies, mitogen panel (CRP not always elevated!)
- EMG, MRI, muscle biopsy
- Clinical associations
- Highly associated with malignancy – workup includes age-appropriate malignancy screen!
- Major subtypes:
- Classic dermatomyositis
- Chronic-onset symmetric proximal weakness with classic cutaneous findings (Heliotrope rash, Gottron’s papules, shawl sign, nail changes etc)
- Associated with ILD in 25% cases
- Anti-synthetase antibody syndrome
- Symmetric proximal weakness, ILD, mechanic’s hands, Raynaud’s phenomenon, arthritis, fever
- Often anti-Jo-1 positive
- Immune-mediated necrotizing myopathy
- Rapidly progressive, symmetric proximal weakness with high CK
- Often associated with HMGCR Ab+ which is often associated with statin use
- You can develop statin-associated muscle adverse events at any time, even if you have been on the medication for years!
- Inclusion body myositis
- MDA5 dermatomyositis
- Associated with rapidly progressive ILD (these patients often need lung transplant), classic cutaneous findings, but less muscle involvement
- Classic dermatomyositis
- Investigations and diagnosis



Leave a comment