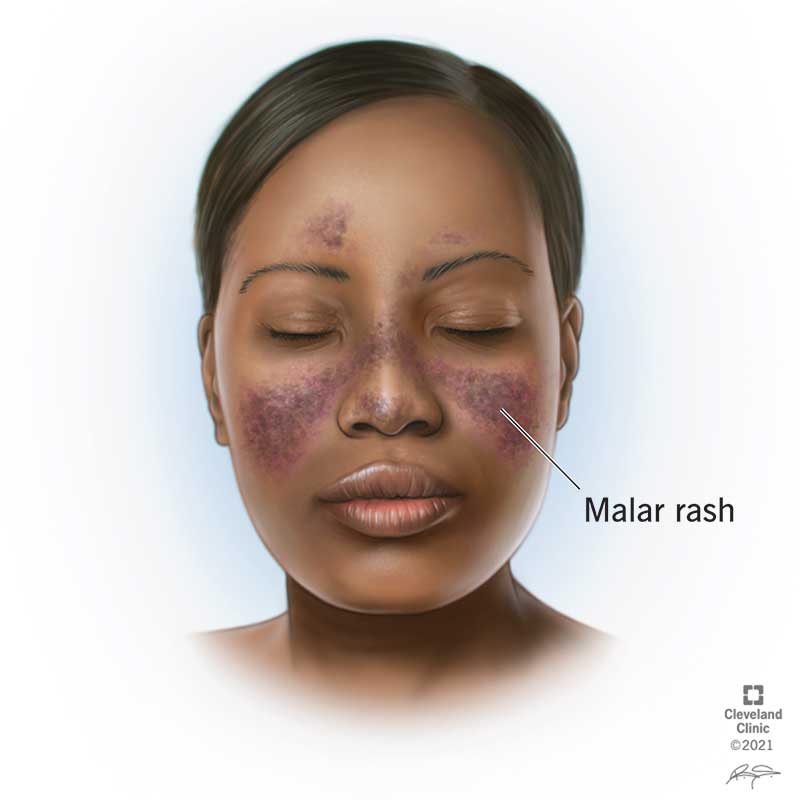
In the second session of this case, we discovered the secondary cause of ITP in our patient with undetectable platelets and elevated PTT due to lupus anticoagulant – new diagnosis of SLE, manifesting in an unusual presentation without the stigmata we look for in our med school illness script (no rash, no arthritis, no ulcers).
Here are some of the key teaching takeaways (Didactic slides):
- ACR/EULAR criteria or SLICC criteria are used to support diagnosis
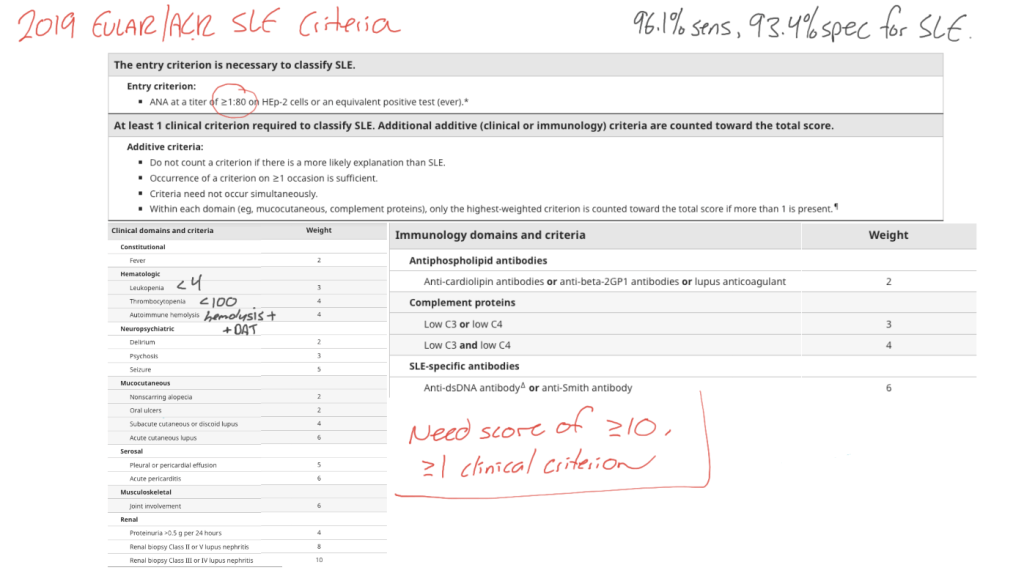
- Note the different entry criterion cutoffs for ANA in the immunofluorescence assay (1:80) vs ELISA assay (~2).
- In conceptualizing the ANA titre, the ratio shows the dilution to which the fluorescence remains positive (essentially, how much diluent needed to wash out a positive result – allowing us to infer the concentration of antibody present). Thus 1:20 is a weaker positive than 1:80, and 1:160 is a stronger positive than 1:80.
- Our patient’s ELISA of 30 (recalling that ELISA 2 ~= IF 1:80) suggests VERY active disease.
- All patients with lupus found to have active urine (proteinuria, hematuria) must have further investigations (including renal biopsy if needed) to rule out lupus nephritis, as some classes of lupus nephritis require aggressive immunosuppression!
- We discussed challenges of acquiring a renal biopsy in a patient with no platelets (as we target PLT > 50 for this procedure). In our case, we had to wait for days for immunosuppression to set in, and ended up using transient PLT increases after IVIG to time the biopsy. Other options including eltrombopag and rituximab are also considered.
- For this patient with positive lupus anticoagulant Ab (B2GP1, anticardiolipin) and functional testing (DRVVT, mixing study with lupus anticoagulant insensitive reagent), we must differentiate between antibody positivity and anti-phospholipid antibody syndrome (APLAS) – management is DIFFERENT
- APLAS diagnosis requires: Positive lab findings (DRVVT + specific Ab positive on >1 occasion at least 12 weeks apart) and clinical findings (VTE/arterial thrombosus, microvascular thrombosis eg APLA nephropathy/skin findings, pulmonary hemorrhage, obstetric events eg miscarriage/placental insufficiency/preeclampsia)
- Management for APLAS requires treatment of the acute thrombosis with heparin, followed by maintenance warfarin (no DOACs)
- Management for triple positive antiphospholipid Ab without APLAS diagnosis is thromboprophylaxis with ASA 81 mg po daily (EULAR 2019).
Thanks for your attention, I hope this session was helpful!



Leave a comment