Hey everyone,
Some pearls from today’s teaching:
Resources
- Bloody Easy Coagulation handbook – coagulation pathway, anticoagulation basics, approach to abnormal coagulation tests
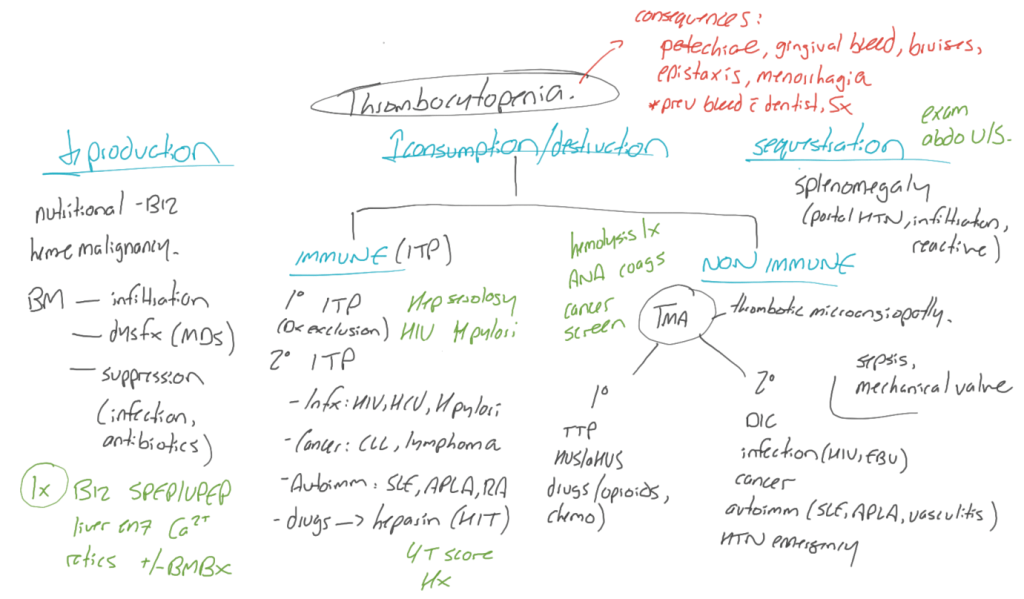
Approach to thrombocytopenia
- Clinical evaluation should include:
- History: Mucocutaneous bleeding, constitutional symptoms, PMHx (cancer, HIV, autoimmune disease), medications (anticoagulants)
- Physical: Vitals, evidence of bleeding (mucous membranes, epistaxis, petechiae/purpura), lymphadenopathy, hepatosplenomegaly
- Indications for platelet transfusion (Canadian Blood Services, AABB/ICTMG systematic reviews):
- PLT < 100 neuraxial surgery, head trauma/CNS hemorrhage
- PLT < 50 major non-neuraxial surgery, epidural anesthesia/lumbar puncture
- PLT < 30 therapeutic anticoagulation that cannot be stopped
- PLT < 20 percutaneous procedures other than LP/epidural anesthesia
- PLT < 10 for any non-immune thrombocytopenia (prophylaxis against spontaneous ICH)
- For ITP – “case specific” – “one dose, for life-threatening bleeding only and consult a hematologist”
Approach to isolated PTT elevation
- Represents a problem with the intrinsic pathway
- What causes elevated PTT?
- Congenital: Factor 8 and 9 (Hemophilia A and B) > vWD with low factor 8, factor 11
- Acquired:
- Factor inhibitor (commonly against factor 8)
- Non-specific inhibitors
- Heparin/DOAC
- Lupus anticoagulants targetting coagulation proteins bound to phospholipids – LA are antiphospholipid Ab that interfere with lab assays for clotting, do not represent increased bleeding risk and in fact increase risk of thrombosis.
- How to investigate:
- Rule out heparin/DOAC
- Assess for lupus anticoagulant
- DRVVT (snake venom enzymes activate central pathway factor 5 and 10, which excludes any deficiency/specific inhibitors of intrinsic pathway factors, thus allows you to assess for assay interference due to LA).
- Screening test uses a reagent with low phospholipids, which should be neutralized due to LA – thus clotting time increases.
- Subsequent confirmatory test uses a reagent with high phospholipids, which should not be fully neutralized – thus clotting time decreases.
- Can do a mixing study (similar to below, but uses a PTT lupus anticoagulant insensitive reagent with phospholipid substrates that are not neutralized by LA in the assay – will see normalization of the PTT)
- DRVVT (snake venom enzymes activate central pathway factor 5 and 10, which excludes any deficiency/specific inhibitors of intrinsic pathway factors, thus allows you to assess for assay interference due to LA).
- Mixing studies – 50:50 mix of normal plasma and patient’s sample. If aPTT corrects on mixing -> factor deficiency. If aPTT does not correct -> inhibitor. If there is partial correction, possibly elements of both inhibitor and deficiency. Can then go on to get specific factor levels (generally 8 and 9).




Leave a comment