Thanks Dr Reynolds!
Here is a summary of physical exam findings in aortic regurgitation, characterization of the JVP and interpretation of abnormal JVP waveforms
Aortic regurgitation
The murmur – decrescendo early-diastolic blowing murmur, best heard on the left lower sternal border (around 3-4th intercostal space) produced by the regurgitant blood jet after the aortic valve “closes”
**Improve yield by sitting the patient upright, leaning forward, and in full expiration (brings heart forward to chest wall)
**Murmur increased with isometric hand grip to increase afterload and increase regurgitant flow.
May be accompanied by Austin Flint murmur (functional mitral stenosis 2/2 AR jet preventing the anterior leaflet of the MV fully opening – producing a mid to late diastolic murmur.
Other findings caused by a widened pulse pressure (increased SBP due to compensatory increased stroke volume + decreased DBP due to retrograde flow)
Examples:
- Corrigan’s pulse (bounding carotid pulse with rapid diastolic collapse)
- Water hammer pulse detected by lifting the patient’s arm and palpating at radial/ulnar/brachial arteries
- MANY other signs where pulsation is detected as a consequence of the wide pulse pressure (Quincke’s capillary pulse, head bob (De Musset), uvula pulsation (Muller’s), retinal artery pulsation (Becker) etc – see the article
Jugular venous pulsation
Neck vein exam – Stanford Medicine 25
- JVP vs carotid
- JVP is biphasic vs carotid monophasic
- JVP changes with position (sinks when you raise head of the bed)
- JVP changes with respiration (decreases with inspiration)
- JVP is non-palpable
- JVP will increase with RUQ pressure
- Features to report:
- The height above sternal angle (at 30 degrees)
- The waveform
- Response to abdominal pressure (positive abdominojugular/hepatojugular finding is a JVP that remains increased over >4cm after 10 seconds of abdominal pressure – a normal response would be transient increase of the JVP with pressure (increased preload) and then decrease as the RV appropriately processes the bolus)
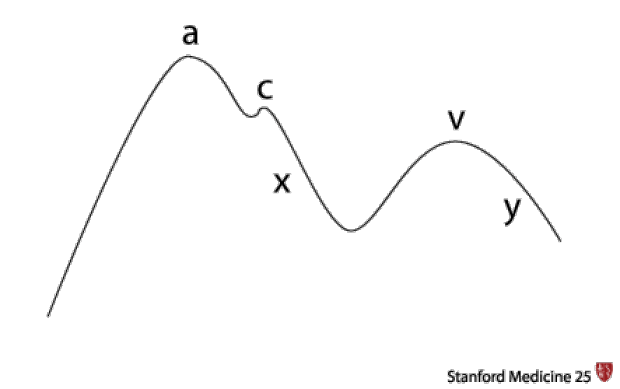
- Jugular venous waveform components:
- A wave due to atrial contraction
- C wave due to ventricular contraction with tricuspid bulging back into RA (you won’t see this clinically)
- X descent due to atrial relaxation
- V wave due to atrial venous filling
- Y descent after the tricuspid opens and the ventricles fill
- Abnormalities in jugular venous waveform:
- Large a wave
- Resistance to right atrial emptying (eg tricuspid stenosis, pulmonary hypertension)
- Atrium contracts against a closed tricuspid eg AV dissociation (third degree heart block, VTach)
- No a wave – no atrial contraction – atrial fibrillation
- Elevated v wave
- Resistance to atrial filling eg due to the backward jet of tricuspid regurgitation
- Absent v wave -> “the patient is dead”
- Large a wave




Leave a comment